Understanding Dry Needling
A primer on the procedure at the center of this reimbursement guide.
What is Dry Needling?
Dry needling is a therapeutic technique performed by skilled physical therapists. It involves inserting a thin, solid filiform needle into the skin and muscle directly at a myofascial trigger point. These trigger points are taut bands of skeletal muscle that can cause pain, tenderness, and limit range of motion.
Who Orders It and Why?
Physicians, such as primary care providers, physiatrists, or orthopedic surgeons, typically order physical therapy that may include dry needling. It's prescribed to treat musculoskeletal pain and movement impairments, including conditions like chronic neck pain, back pain, tension headaches, and sports injuries. The goal is to release trigger points, reduce pain, and restore normal muscle function.
Key Distinction
Unlike acupuncture, which is based on traditional Chinese medicine and aims to restore the flow of "qi" or energy, dry needling is a modern, science-based intervention rooted in Western medicine. Its primary focus is on treating specific neuromuscular trigger points to relieve pain and improve movement.
Mastering the Codes: A Deep Dive into Dry Needling CPTs
Using the right code is non-negotiable for payment. Here's a detailed look at the two codes specific to dry needling.
CPT 20560: The Base Code
Official Description: Needle insertion(s) without injection(s); 1 or 2 muscles.
When to Use It: Use this code for any dry needling session where one or two distinct muscles are treated. This is the primary, standalone code for a basic session. It should only be billed once per patient encounter.
CPT 20561: The Add-On Code
Official Description: Needle insertion(s) without injection(s); 3 or more muscles.
When to Use It: This is an add-on code. It can only be used in conjunction with CPT 20560. Bill both 20560 and 20561 when the session involves treating three or more distinct muscles.
Common Billing Errors to Avoid
- Billing 20561 Alone: Never bill the add-on code 20561 without the primary code 20560 on the same claim. It will be denied.
- Incorrect Units: Both 20560 and 20561 are billed with only one unit per session, regardless of how many needles are inserted. Do not bill multiple units.
- Improperly Unbundling Manual Therapy (CPT 97140): If you perform manual therapy on the *same muscles* you are needling, payers will almost always bundle the services and deny 97140. To bill 97140 on the same day, it must be performed on a distinctly separate anatomical site, and your documentation must clearly support the medical necessity for both procedures.
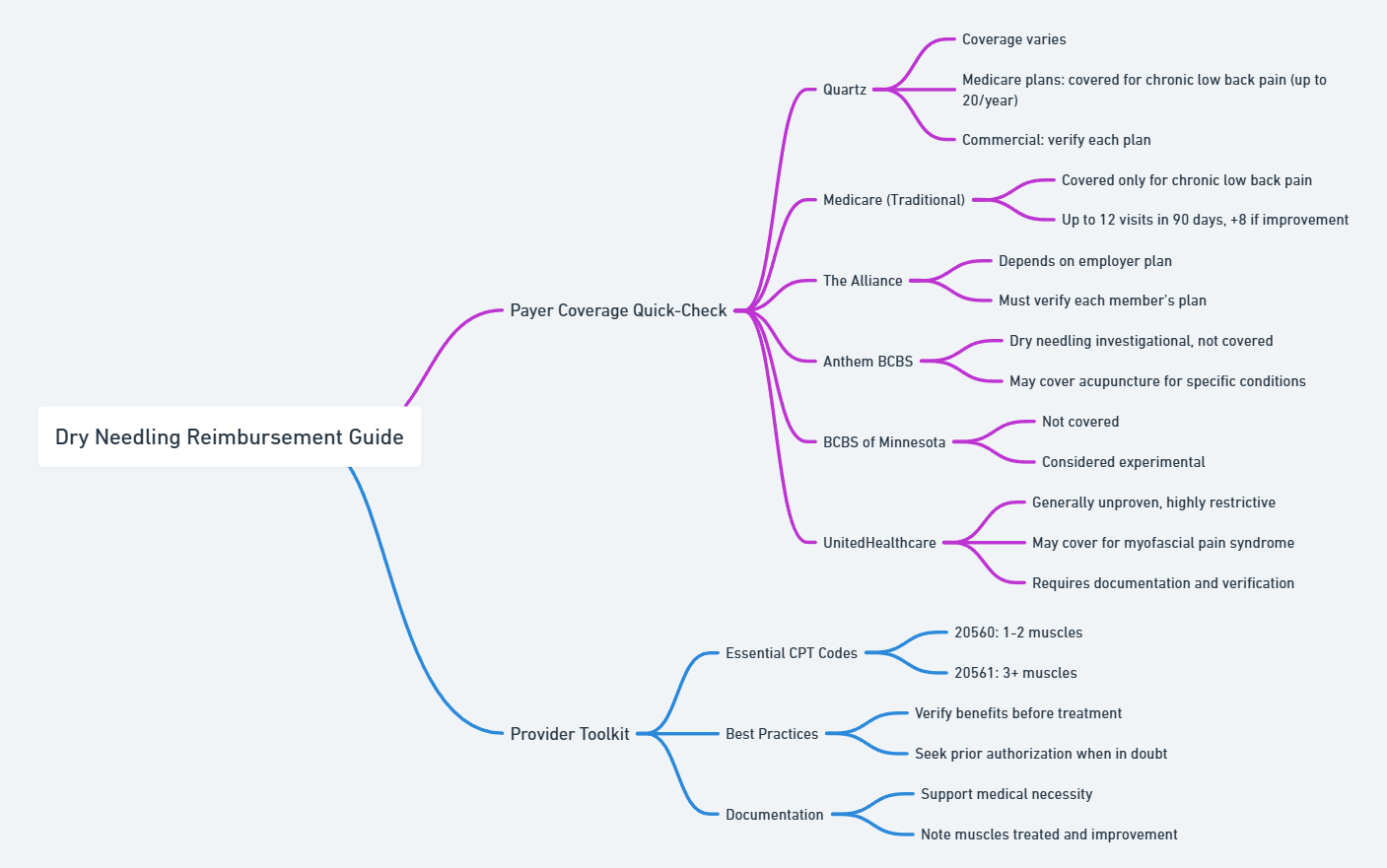
Payer Coverage Quick-Check
Click on a payer card below for detailed policy information.
Reimbursement Mindmap
A visual guide to the decision-making process for dry needling reimbursement.